Irritable Bowel Syndrome (IBS) is a prevalent condition that affects the digestive system. It causes symptoms like constipation, pain, and bloating. This article delves into the symptoms, causes, and ways to manage IBS. This article sheds light on the various facets of Irritable Bowel Syndrome, offering insights into its symptoms, causes, and the multiple methods available for its treatment and management.
What is Irritable Bowel Syndrome (IBS)?
Understanding the basics of IBS. Irritable Bowel Syndrome, commonly abbreviated as IBS, is a chronic condition affecting the digestive system, specifically the colon. It is not synonymous with other digestive disorders like cancer. People diagnosed with IBS experience discomfort in their abdomen, gas, and changes in bowel habits.
Prevalence in the United States and Globally
Description: How common is IBS? Research indicates that a considerable portion of the global population, especially in the United States, is affected by IBS. Women tend to have a higher predisposition to the condition, with age and family history being prevalent.
Symptoms of IBS
Recognizing the common signs of IBS. People with IBS often complain of constipation or diarrhea. Bloating, gas, and abdominal pain are almost omnipresent. Some might notice mucus in their stool, while others may experience weight loss or vomiting.
Emotional and Psychological Impacts
Description: Beyond the physical. It’s noteworthy that IBS doesn’t just affect the body. Anxiety and depression are common among IBS patients. Consistent discomfort and unpredictability of bowel movements can lead to heightened stress levels.
Causes and Risk Factors
What might instigate IBS? While the exact cause of IBS remains unclear, several triggers have been identified. Changes in the digestive tract’s nerves, infections, and bacterial imbalance in the intestines can set off IBS. Changes in diet or food can also be a cause, as well as an overly sensitive colon or immune system reaction.
Risk Factors and Genetic Predisposition
Description: Who is more likely to get IBS? Family history is pivotal. If your family has a history of IBS, your risk escalates. Furthermore, age plays a role; younger adults are more prone. Additionally, psychological factors like anxiety or past trauma can increase susceptibility.
Diagnosing and Treating IBS
How is IBS identified? Doctors review the patient’s symptoms and medical history for a concrete diagnosis. Tests are often conducted to rule out other diseases. It’s essential to differentiate IBS from other digestive disorders, especially those with similar symptoms like stomach infections or, in rare cases, cancer.
Treatment Options and Lifestyle Changes
Description: Alleviating the symptoms. Treatment for IBS often revolves around alleviating symptoms. Dietary changes, medication, and managing stress are pivotal. Remedies can range from drugs that control diarrhea or constipation to those that ease abdominal pain. Lifestyle changes, including a balanced diet and regular exercise, can be incredibly beneficial.
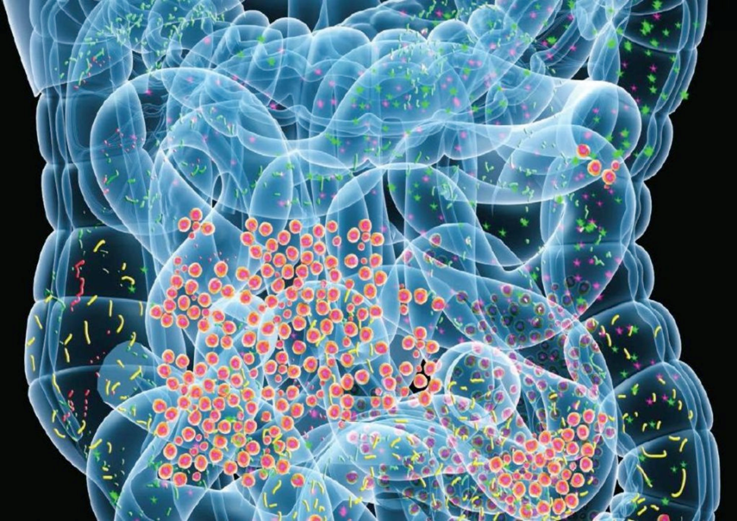
The Role of Probiotics in Managing IBS
Maintaining a balanced gut microbiome can be instrumental in alleviating the symptoms of IBS. Recent studies indicate that probiotics might benefit those grappling with digestive system issues.
Recognizing the Need for Probiotics
Determining when your gut needs extra support. Certain signs can hint at the need for probiotics. From frequent digestive disturbances to a weakened immune system, understanding these signals can pave the way for better gut health and potentially reduce IBS symptoms.
Probiotics, Prebiotics, and Digestive Tract Health
Description: Harnessing the power of beneficial bacteria. A balanced gut microbiome can significantly reduce the risk of digestive tract issues. Introducing probiotics and prebiotics into one’s diet can promote a harmonious gut environment, often leading to improved digestive processes and decreased discomfort.
Achieving Stomach Relief with Optimized Probiotics
Description: The new age of targeted probiotic solutions. The advent of microbiome-optimized probiotics has revolutionized gut health. These tailored solutions provide stomach relief by targeting specific issues, ensuring that the body receives the right type of beneficial bacteria where it’s most needed.
By incorporating this section, readers gain insight into an alternative yet scientifically backed approach to managing IBS symptoms. It allows them to consider a broader range of solutions and underscores the importance of gut health in overall well-being.
Living with IBS
Making daily life more comfortable. People with IBS often need to monitor their diet closely. Foods that exacerbate symptoms are best avoided. Regular consultation with a doctor or healthcare professional is vital. Being open about the condition is equally important, as emotional and social support can be invaluable.
Seeking Support and Additional Information
Description: You’re not alone. There are several IBS-focused support groups, both online and offline. These groups offer a platform to share experiences, gather information, and seek advice. Research continually offers new insights into IBS, and staying updated can make life with the condition more manageable.
Conclusion
In conclusion, Irritable Bowel Syndrome is a prevalent condition that affects many worldwide. While it can be challenging to live with, understanding the situation, its symptoms, and causes, coupled with effective management and a supportive community, can significantly enhance the quality of life for those diagnosed.
What is Irritable Bowel Syndrome (IBS)?
IBS is a chronic condition affecting the digestive system, particularly the colon, causing symptoms like bloating, gas, constipation, and diarrhea.
Is IBS the same as colon cancer or other digestive diseases?
IBS is not the same as colon cancer or other digestive diseases. It’s crucial to consult a doctor for a precise diagnosis.
What are the primary symptoms of IBS?
Common symptoms include abdominal pain, bloating, constipation, and diarrhea. Some patients may also notice mucus in their stool.
PASSOS, Maria do Carmo Friche, & MORAES-FILHO, Joaquim Prado. (2017). INTESTINAL MICROBIOTA IN DIGESTIVE DISEASES. Arquivos de Gastroenterologia, Epub July 06, 2017.https://dx.doi.org/10.1590/s0004-2803.201700000-31