Buckle up, ladies! Have you ever felt like a completely different person at various times of the month? Mood swings, hunger pangs, and drastic energy shifts are your body’s unique way of signaling various menstrual cycle phases. Understanding these stages demystifies your monthly metamorphosis and can empower you to work harmoniously with your body’s natural rhythms. This comprehensive guide will take you through the winding path of menstrual cycle phases, equipping you with knowledge that can revolutionize how you navigate those roller-coaster days each month. It’s time to decode the menstrual mystery!
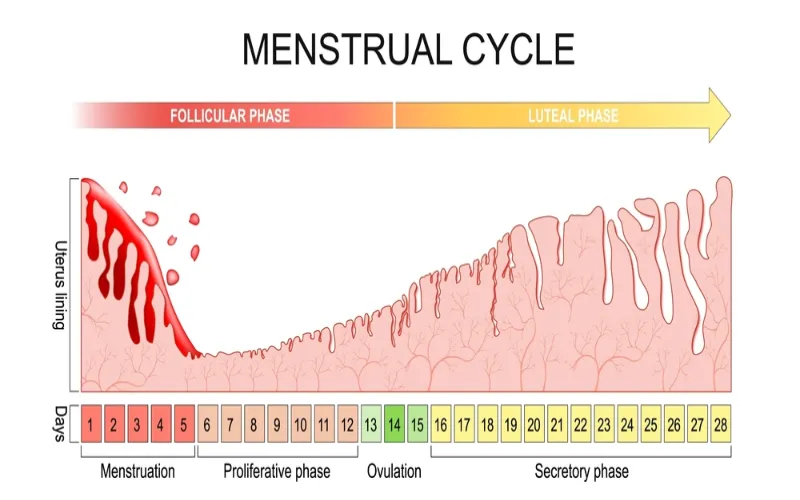
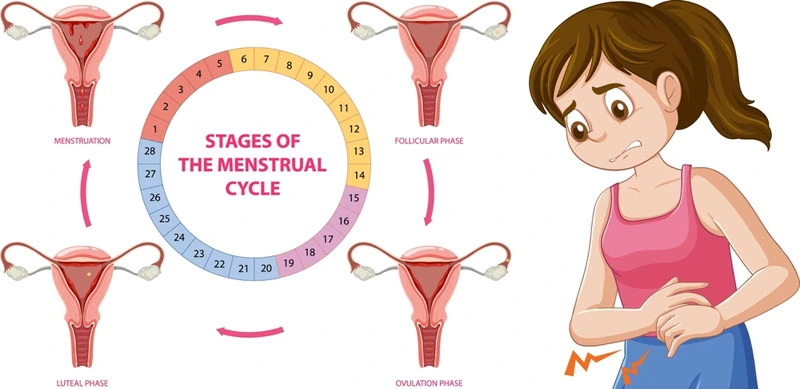
The menstrual cycle is composed of four phases:
1. Menstrual phase – shedding of the uterine lining lasting from day one to day five;
2. Follicular phase – estrogen levels rise, causing the endometrium to grow and follicles in the ovaries to develop until one releases a mature egg;
3. Ovulation – egg release around day 14 in a 28-day cycle;
4. Luteal phase – progesterone levels rise to prepare the uterine lining for pregnancy, and if no fertilization occurs, hormones drop, leading to menstruation. By understanding these phases and tracking changes in your body’s cycles over time, you can better understand your fertility and overall health.
Defining the Menstrual Cycle
The menstrual cycle is a remarkable process in women’s bodies, vital to their reproductive health. It is a cyclical series of events that prepares the body for potential pregnancy each month. Essentially, the menstrual cycle refers to the period from the first day of one period until the first day of the next period.
On average, a menstrual cycle lasts around 28 days, although it can vary from woman to woman and even from month to month. Some women have shorter cycles of about 21 days, while others may experience longer cycles of up to 35 days. It’s important to note that variations in cycle length are generally considered normal as long as they fall within these ranges.
During the menstrual cycle, several distinct phases occur, each driven by hormones released by the pituitary gland and ovaries. These hormonal fluctuations are crucial in preparing the body for pregnancy and regulating physiological changes.
The Role of Hormones
Hormones act as messengers within our bodies, orchestrating various processes and ensuring everything runs smoothly. Concerning the menstrual cycle, several key hormones come into play:
- Follicle-Stimulating Hormone (FSH): At the start of the menstrual cycle, FSH is released by the pituitary gland. Its primary function is to stimulate follicles in the ovaries to develop.
- Estrogen: As follicles grow, they produce estrogen, an essential hormone that thickens and nourishes the uterine lining called endometrium. Estrogen levels rise steadily throughout the follicular phase.
- Luteinizing Hormone (LH): As estrogen levels increase, the pituitary gland releases LH. A surge in LH triggers ovulation, which marks the release of a mature egg from one of the ovaries.
- Progesterone: After ovulation, the ruptured follicle transforms into a structure called the corpus luteum, which produces progesterone. Progesterone prepares the uterine lining for potential pregnancy by thickening it further and maintaining its integrity.
Think of FSH as an orchestra’s conductor, initiating the menstrual cycle’s initial stages. Estrogen takes on the role of building up and nurturing the stage (the endometrium) for a potential performance (pregnancy). Then, LH steps in as the spotlight operator, signaling when it’s time to release the main act (the egg). Finally, progesterone is the caretaker, ensuring everything is in place for a successful show (implantation).
These hormones work intricately together, creating a delicate balance throughout different phases of the menstrual cycle. If fertilization doesn’t occur during this cycle, hormone levels drop, leading to menstruation – the shedding of the uterine lining.
Having explored the defining aspects of the menstrual cycle and delved into the roles hormones play in this process, we can now explore specific phases in more detail.
The Start: Menstrual Phase
The journey of the menstrual cycle begins with the menstrual phase, also known as the start of the cycle. This phase marks the shedding of the uterine lining, resulting in vaginal bleeding. It is a response to hormonal changes when pregnancy does not occur.
During this phase, which typically lasts for three to seven days, the body releases prostaglandins, hormones that cause the uterus to contract, resulting in cramps. These contractions help expel the old uterine lining through the cervix and out of the body.
You might notice changes in your energy levels and mood as menstruation begins. Some individuals may experience fatigue and decreased physical stamina during this time. Hormonal fluctuations can also contribute to mood swings, irritability, or feeling more emotionally sensitive than usual.
It is important to listen to your body’s needs during this phase. Resting when needed and engaging in gentle exercises like yoga or walking can help alleviate discomfort while supporting overall well-being.
Your bleeding pattern may vary from light to heavy flow throughout your period. It’s normal to be heavier on the first few days and then gradually taper off. Comfortable menstrual products like menstrual cups, reusable pads, underwear designed for periods, sanitary napkins, or tampons are widely used to absorb menstrual blood during this phase.
For instance, Sarah experiences a heavier flow at the beginning of her period and opts for menstrual cups as they provide longer wear without leakage. On the other hand, Maya uses reusable cloth pads both for comfort and environmental reasons.
Now that we have explored the start of the menstrual phase and its characteristics let’s delve into symptoms experienced during this time and self-care strategies that can make this phase more manageable.
Learn More: Purple Period Blood Explained: Causes & Treatment
Symptoms and Self-care
During menstrual, you may experience various symptoms that vary widely between individuals. These symptoms are the body’s response to hormonal changes and the shedding of the uterine lining.
Think of it as a unique orchestration occurring within your body. Just like each musical score has its variations, your menstrual symptoms may differ monthly.
Common symptoms during this phase include abdominal cramps, lower back pain, bloating, breast tenderness, mood swings, fatigue, and headaches. For some individuals, these symptoms might be mild and manageable, while for others, they can be more intense and disruptive. Listening to your body and providing self-care is crucial during this time.
Emma experiences severe abdominal cramps each month that impact her daily activities. To manage this discomfort, she applies a hot water bottle to her abdomen and takes over-the-counter pain relief medication as necessary.
Practicing self-care is essential to enhance your well-being during the menstrual phase and alleviate symptoms. You can try incorporating relaxation techniques such as deep breathing exercises or engaging in activities that bring joy and help release stress.
Nutrition also plays a role – consuming balanced meals with plenty of fruits, vegetables, whole grains, and healthy fats can provide necessary nutrients and minimize discomfort. Staying hydrated by drinking sufficient water throughout the day can also help with bloating.
Now that we have covered the symptoms experienced during the menstrual phase and explored self-care strategies to manage them effectively, let us move on to understanding the next phase of the menstrual cycle – the follicular phase.
Egg Preparation: Follicular Phase
The menstrual cycle is a complex process that involves various phases, each with specific functions and hormonal changes. The follicular phase marks the beginning of the cycle and is responsible for egg preparation in anticipation of ovulation. This phase typically lasts from the first day of menstruation until ovulation occurs.
During the follicular phase, the pituitary gland releases two essential hormones: follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FSH plays a crucial role in stimulating the growth of follicles in the ovaries, while LH helps facilitate the maturation of these follicles.
To better understand this phase, consider an example: Imagine your ovaries as a garden where each follicle represents a potential seed. At the start of the menstrual cycle, multiple follicles grow under the influence of FSH. However, only one follicle eventually becomes dominant and matures, thanks to its ability to respond more effectively to FSH.
As this dominant follicle develops, it produces estrogen, a hormone that supports the growth and thickening of the uterus lining known as the endometrium. This increase in estrogen triggers a negative feedback loop that suppresses FSH production, preventing other follicles from maturing further.
Understanding Ovulation
Ovulation is a vital event that occurs during the menstrual cycle, usually around day 14 in a 28-day cycle. It involves the release of a mature egg from the ovary into the fallopian tube, where it awaits fertilization by sperm.
Let’s compare ovulation to releasing a beautiful butterfly into a garden. An egg emerges from its protective follicle during ovulation as this butterfly flutters out of its cocoon to explore new possibilities.
The luteinizing hormone (LH) surge triggers the final maturation and release of the egg. LH levels spike, signaling to the dominant follicle that it’s time to rupture and release the mature egg into the fallopian tube.
Once released, the egg travels through the fallopian tube, propelled by tiny hairs called cilia. This is the prime time for fertilization if sperm is present in the reproductive tract. The egg can survive in the fallopian tube for up to 24 hours after ovulation, waiting for sperm to facilitate fertilization. If fertilization doesn’t occur within this timeframe, the egg will disintegrate and be expelled with the next menstrual cycle.
It’s important to note that ovulation may not always occur on day 14, as cycle lengths can vary. Stress, illness, hormonal imbalances, or certain medical conditions can impact ovulation timing. Tracking your menstrual cycle and observing changes in cervical mucus or using ovulation predictor kits can help identify when you are most likely to ovulate.
Now that we’ve explored the journey of an egg from its preparation during the follicular phase to its release during ovulation, we will delve into the subsequent phase known as the luteal phase.
- Ovulation is a crucial event in the menstrual cycle, where a mature egg is released from the ovary into the fallopian tube, waiting for fertilization. It’s essential to understand that the timing of ovulation may vary due to various factors like stress, medical conditions, hormonal imbalances, and more. Tracking menstrual cycles and identifying changes in cervical mucus or using ovulation predictor kits can facilitate recognizing ovulation.
Learn More: Duration of Menopause: What Every Woman Should Know
After Ovulation: Luteal Phase
Once ovulation occurs and an egg is released from the ovary, the body enters the luteal phase of the menstrual cycle. This phase typically lasts around 12-16 days and is characterized by significant hormonal changes that prepare the uterus for a potential pregnancy.
During this phase, levels of progesterone rise, stimulating the thickening of the uterine lining (endometrium). The purpose of this thickening is to provide a nurturing environment for a fertilized egg to implant itself and develop into a pregnancy. If fertilization does not occur, progesterone levels drop, triggering the start of menstruation.
It’s important to note that while the luteal phase duration is relatively consistent among women, it can vary slightly from person to person. Tracking your monthly cycles can help you determine the length of your luteal phase and better understand your unique reproductive patterns.
It’s common to experience several physical and emotional changes during this phase. Many women may notice breast tenderness, bloating, mild cramping, and heightened sensitivity during this time. Additionally, some individuals may experience mood swings or feel more tired than usual due to hormonal fluctuations.
The luteal phase is crucial for maintaining a healthy menstrual cycle, but it is also essential in identifying any potential abnormalities or irregularities.
Possible Changes and Abnormalities
While variations in menstrual cycles are generally considered normal, certain changes or abnormalities during the luteal phase might warrant further attention. It’s important to be aware of these signs to address any potential underlying issues:
- Short Luteal Phase: A luteal phase lasting less than 10 days could indicate insufficient progesterone production, making it harder for a fertilized egg to implant or sustain a pregnancy. Consulting with a healthcare provider can help identify the cause and explore potential solutions.
- Irregular Menstrual Periods: Significant variations in cycle length or inconsistent timing of menstruation may affect the duration of the luteal phase. Irregular periods can be caused by various factors such as stress, hormonal imbalances, polycystic ovary syndrome (PCOS), or certain medical conditions. Identifying the underlying cause is crucial for maintaining reproductive health.
- Premenstrual Syndrome (PMS): Some individuals experience heightened physical and emotional symptoms during the premenstrual phase of their menstrual cycle, which overlaps with the latter part of the luteal phase. These symptoms may include mood swings, bloating, breast tenderness, headaches, and fatigue. While mild PMS symptoms are common and generally resolve with menstruation, severe or disruptive symptoms may require medical intervention.
- Hormonal Imbalances: Fluctuations in hormones during the luteal phase can significantly impact overall well-being. Conditions like premenstrual dysphoric disorder (PMDD) or hormonal imbalances can lead to intense physical and emotional changes that affect daily life. Seeking guidance from a healthcare provider can help manage these imbalances effectively.
If you notice any concerning changes or abnormalities during your luteal phase, it’s always wise to consult a healthcare provider for a thorough evaluation. They can guide you through appropriate diagnostic tests, offer personalized advice, and provide treatment options.
What lifestyle factors or interventions may impact the duration or severity of each phase of the menstrual cycle?
Lifestyle factors such as stress, sleep, exercise, and diet can impact the duration and severity of each menstrual cycle phase. High levels of chronic stress may lead to irregular cycles or even amenorrhea. Adequate sleep is essential for maintaining balanced hormones and a healthy menstrual cycle. Regular exercise has been shown to reduce menstrual pain and improve overall cycle regularity. A well-balanced diet with sufficient nutrients like iron, calcium, and omega-3 fatty acids can help support hormonal balance and alleviate symptoms.
Can the length or characteristics of a woman’s menstrual cycle change over time?
Yes, the length and characteristics of a woman’s menstrual cycle can change over time. Age, hormonal fluctuations, stress levels, weight or exercise patterns, and certain medical conditions can influence the menstrual cycle.
What signs or symptoms might indicate a problem with one of the menstrual cycle phases?
Some signs or symptoms that might indicate a problem with one of the menstrual cycle phases include irregular periods, severe pain or cramping, excessively heavy or light flow, prolonged bleeding, and absence of menstruation. These symptoms could indicate underlying issues such as hormonal imbalances, polycystic ovary syndrome (PCOS), endometriosis, or thyroid disorders.
What happens to hormone levels during each phase of the menstrual cycle?
During the menstrual cycle, hormone levels fluctuate in four phases: the menstrual phase, follicular phase, ovulation phase, and luteal phase. In the menstrual phase, estrogen and progesterone levels drop, leading to the shedding of the uterine lining. As the follicular phase begins, estrogen rises, stimulating the maturation of an egg in the ovary. Ovulation occurs when a luteinizing hormone (LH) surge triggers the mature egg’s release.
How long does each phase of the menstrual cycle typically last?
The duration of each phase of the menstrual cycle can vary for different individuals. Still, on average, the follicular phase typically lasts around 11 to 21 days, while the luteal phase lasts about 12 to 16 days. These figures are based on a study by the American College of Obstetricians and Gynecologists. However, it is important to note that individual variations and hormonal fluctuations can cause these durations to differ.